If asymptomatic cases of Covid-19 are as infectious as symptomatic cases, then 94% of the student population will get infected during the first term. One third of infected students will be in their first year, and reducing face-to-face teaching is likely to be the single most effective intervention to address it.
Those are some of the main findings from a newly published pre-print from a team at the University of Bristol. They’re not predictions – for absolute clarity those figures assume few controls or interventions – and as it’s a pre-print the work has not been certified by peer review. But the work is fascinating given what we know about the way part of it might have influenced Scientific Advisory Group for Emergencies (SAGE) advice.
Back in July you may well remember that we did a write up of discussions held by SAGE on universities. Specifically, we noted that its Scientific Pandemic Influenza Group on Modelling (SPIMO) had looked at some initial modelling of how the virus might spread in a couple of universities but that more would help to identify “commonalities and generalisable insights”. “More” never came.
What worried us at the time was the assertion that students moving from their family households to set up new, temporary households during term time, “will want to return to their family households at the end of terms”. That sounded like assumptions about a “boarding school” model to us, rather than the reality of commuting (and mixing) for many students, and a more hidden hybrid of students that are indeed residential but go “home” almost every weekend. Was SPIMO basing its advice to SAGE and therefore advice to DfE and then universities on flawed assumptions about students?
Some headlines
The new pre-print looks at one of the two SPIMO-mentioned studies, this one from Bristol itself – and there’s also a separate “rapid review” of modelling studies. Overall they develop a “new, detailed epidemic model” based on UK student data, and evaluate the things you could do to intervene, “testing, contact tracing, quarantine strategies, and other non-pharmaceutical interventions”.
The analyses provide some interesting recommendations to policy makers and the higher education sector:
- “Multiple interventions” will be required to enable universities to respond quickly to any evolving increases in cases, which include reducing peoples’ contacts (within residences and across the university community), effective testing (!), tracing and quarantine of individuals.
- Limiting contacts via reduced face-to-face teaching was the single most effective control option.
- Students and staff will need to closely adhere to the national guidance around social distancing and hand washing, and will need clear advice on what to do if they are symptomatic or asked to quarantine to help avoid large number of cases in the university community. But what if they don’t?
- Policies aimed at reducing how many people individuals come into contact with, and the risk of transmission during any face-to-face contacts, are critical. This, it says, could include moving teaching online, social distancing, and the correct use of face coverings. But how much teaching should be moved online?
- If mass testing is used, it needs to be frequent, with persons without symptoms being tested weekly or more often. That’s either very expensive (university organised) or not looking possible right now (government organised).
Contacts
The modelling paper notes that a number of studies have investigated the challenges of reopening campuses, but have looked at fairly isolated campus universities in the US, rather than the more common civic-integrated universities that we have in the UK and elsewhere. It also notes the lack of “realistic mixing patterns” within a university setting that drive transmission in those models.
So what they do here is combine some analysis of (Bristol) student social contact data with a mathematical modelling approach to investigate the impact of re-opening a UK university on transmission. To get there they investigated the dynamics of an epidemic in the student population with limited attempts at stopping it – building in what I would still regard as a generous assumption that symptomatic cases are tested and students start to self-isolate within 48 hours.
Where they guess that asymptomatic cases are half as infectious as symptomatic cases, without interventions or holidays they predict a university-wide outbreak that takes around 4 months to peak. Here first year students drive the early part of the outbreak and experience the highest burden of infection, and by the end of the first term, 5,760 out of 28,000 students have been infected with symptomatic cases, and 880 asymptomatic cases are infectious on the last day of term. More alarming numbers in terms of rapidity of the outbreak are available if, instead, you assume that asymptomatic cases are just as infectious as symptomatic cases.
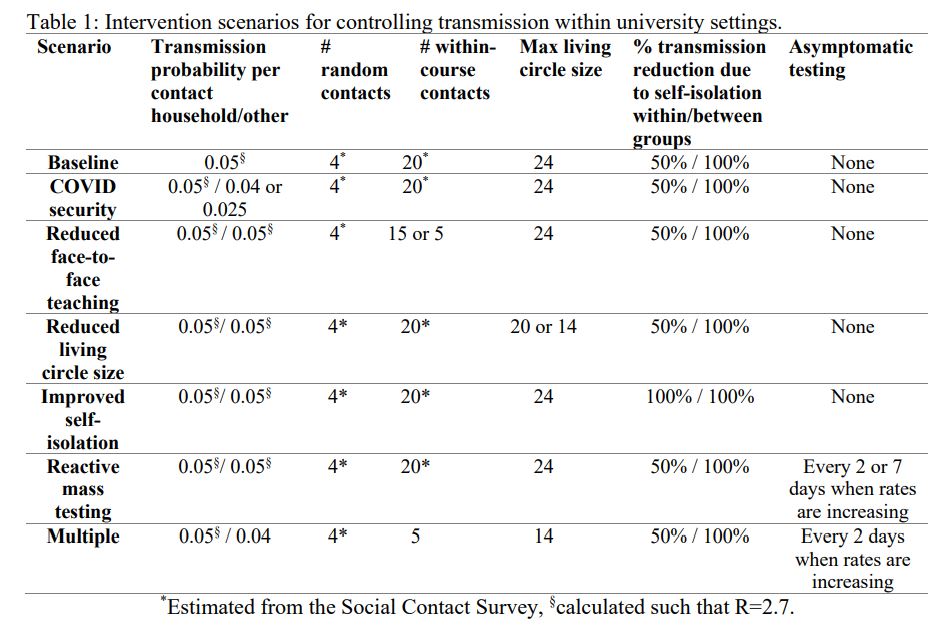
What they then do is examine some specific things that universities could do, and the potential impact of those measures:
- The “baseline conditions” are “business as usual” behaviour within universities with PHE guidelines. This (as noted above) does involve the potentially dangerous assumption that symptomatic cases are tested and moved into self-isolation after an average of 48 hours if test-positive. It also assumes no additional testing for people with no symptoms, and students are assumed to be in living “circles” that are made up of a maximum of 24 students to “reflect existing University of Bristol arrangements”.
- An intervention they call “Covid security” is then modelled by reducing the transmission probability associated with contacts students don’t live with by 25% and 50% to capture the impact of face covering use and social distancing – the classic “Covid secure campus” stuff.
- Another – “reduced face-to-face teaching” – is captured by reducing the number of face-to-face teaching contacts from 20 students to 15 and then 5 students in their model.
- And then “reduced living circles” reflects reducing the number of students sharing facilities within accommodation. In their baseline scenario, they assumed that students were in contact with other students living in the same accommodation, forming household groups up to a maximum of 24 individuals. For accommodation with more than 24 residents, they divided the accommodation population up into “living circles” of 24 students, and to explore the impact of living circle size, reduced the maximum living circle size from 24 to 20 and then 14.
- They simulated scenarios in which all students were tested if the number of test-positive cases in a given week is greater than the previous week, and they go into self-isolation after an average of 2 days. Additional testing is continued until the number of test-positive cases in a given week is less than the previous week. This is the “throw a bag of testing at the wall if you have a little outbreak” strategy.
- And then finally they investigated the impact of each of the above interventions in isolation and then applied sequentially: 25% reduction in transmission due to Covid security, followed by a reduction in face-to-face teaching to 5 study contacts, followed by a reduction in living circles to 24 individuals, reactive mass testing every 2 days if the infection rate on campus should rise, and a reduction in “importation rates” from outside the university population.
It’s face to face teaching
So what did they find? Reducing the number of face-to-face teaching contacts from 20 to 5 other students was the “single most impactful intervention” investigated in terms of the number of students infected by the end of the first term, and the number of infectious students on the last day of term. Once you’re at 5 people in a seminar, is that really better than 15 people on Zoom at a more sensible hour?
On the other hand, reducing the size of “bubbles” (defined here as ”living circles” – or the number of students that share bathroom/kitchen facilities) from 24 to 20 or 14 students was overall the least effective intervention investigated. Overall they found that implementing multiple, layered interventions was able to effectively control transmission in the student population more generally.
The discussion in the paper is where things get really interesting. In this analysis, first year students experienced the highest rates of infection and dominate the early part of the outbreak because of the high levels of mixing in (Bristol’s) halls – what some have called the “landlocked cruise ship” problem. Maintaining social distancing between bubbles within halls, they argue, is paramount for maintaining Covid-19 control – but may be nigh on impossible in practice.
Importantly, this team had limited data on contact with the “location population” (ie Bristolians) and did not include university staff explicitly in the model. “Given the age distribution of students, and the high likelihood of asymptomatic infection”, they say, “staff and surrounding communities are likely to experience higher levels of morbidity than the students themselves”.
They add “although by-and-large students fraternise with students, they do pose some risk to more vulnerable groups within the university such as staff with co-morbidities, or to their local community”, but while that may be true of University of Bristol students, it may for example be less true of, say UWE’s students.
Where’s the modelling?
When you then look across to the rapid review of modelling studies you realise just how little we have in terms of modelling to go on. One paper assesses the impact of opening Cornell’s Ithaca campus and implementing asymptomatic testing (screening), contact tracing, and quarantine measures, compared to having full online/ virtual teaching. Another assesses the impact of testing, screening and isolation/quarantine in a university setting in the US. One looks at the impact of disease transmission amongst freshers on campus when there is a “social bubbling strategy” enforced, and one looked at testing required to detect an outbreak at an early stage in a university campus context in US. And that’s it.
None look at the type of halls a university has (and how many are in PBSA private blocks), none look at the extent of mixing with communities, none address patterns of behaviour when “going home” either regularly or when commuting, none look at how close students live to campus or the local nightlife or the use students make of buses, none address whether students actually do self isolate, none take into account the shambles of testing we have right now, and none look at whether students actually will report symptoms and tell the truth to tracing call handlers. As the rapid review notes:
Most of the models have considered campus universities in the US. In the UK there may be additional considerations. Differences for campus or city integrated universities in terms of mixing with general population are important for importation of infection to the university community, but also spill over of any university outbreaks into the community. However, limited work has been done in this area to date.
There is much uncertainty in the model parameters and the structure of the models, particularly related to how people mix with each other. Student behaviour and mental health under quarantine is important, particularly as many students have small living quarters. Quarantining for students new to university may find isolation particularly lonely and significantly adversely affect mental health – if parents choose to pick up their students for quarantining at home this may drive an increase in community transmission leading to a worse outcome nationally.
And in a revealing nod to that “students at Bristol are probably more likely to be full of people that went to boarding school” assumption again:
Additional risk to the broader population is due to education and accommodation breaks during reading weeks, Christmas and Easter holidays. Requiring students to remain at university during those times is unlikely, and should a substantial number of cases be present in the student population, a large-scale return to home is likely to disperse the infection across the country.
There’s two ways of looking at this.
One would be to say “we’re in a pandemic, everything is new and difficult, and everyone’s doing their best”.
Another would be to say “blimey – the advice that SAGE is giving to the DfE is based on modelling which fails to take into account lots of important things. Why on earth hasn’t more modelling been commissioned and carried out that takes those things into account? Why have we not, as a sector, commissioned some science that involves students who could have pointed out lots of these things? Why don’t we have modelling that uses the good data? Are we all just guinea pigs living through a weird public health experiment and we’ll only really learn at the end of term?”
I’m going with the latter, if that’s OK with everyone.